 Alpha-1 Antitrypsin Deficiency also known as Alpha-1, A1AD or AATD is an inherited, genetic condition that is passed on from generation to generation. As the name suggests it is a deficiency of alpha-1 antitrypsin (AAT) in the bloodstream. AAT is an enzyme produced in the liver to help protect the tissues of the body during infections. The low level of AAT in the blood occurs because the AAT is abnormal and cannot be released from the liver at the normal rate. This leads to a build up of abnormal AAT in the liver that can cause liver disease and a decrease of AAT in the blood that can lead to lung disease.
Alpha-1 Antitrypsin Deficiency also known as Alpha-1, A1AD or AATD is an inherited, genetic condition that is passed on from generation to generation. As the name suggests it is a deficiency of alpha-1 antitrypsin (AAT) in the bloodstream. AAT is an enzyme produced in the liver to help protect the tissues of the body during infections. The low level of AAT in the blood occurs because the AAT is abnormal and cannot be released from the liver at the normal rate. This leads to a build up of abnormal AAT in the liver that can cause liver disease and a decrease of AAT in the blood that can lead to lung disease.
In the early sixties, Dr. Sten Erikkson was working in his home country of Denmark trying to discover why it was that patients who were relatively young were presenting with symptoms of severe Chronic Obstructive Pulmonary Disease (COPD), a term that includes bronchitis and emphysema. Despite rather limited resources at the time, Dr. Eriksson discovered that a group of patients appeared to have low levels of a protein circulating in their blood. He called this protein Alpha-1 Antitrypsin.
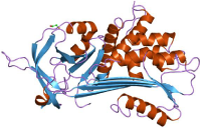
These days researchers tend to call this protein Alpha-1 Proteinase Inhibitor. Here we will call it AAT. This protein is made in the liver, and the levels found in someone normal usually varies between 1.1 grammes / litre and 2.1 grammes / litre of blood. One of the most important jobs this protein carries out is to protect delicate lung tissue against substances released by white blood cells. If we have a chest infection these white cells, called neutrophils, are able to move through cellular walls to kill bacteria and clean up other debris. To do this the neutophil releases an enzyme called neutrophil elastase. This enzyme is able to dissolve Elastin which is the tissue that makes up the structure of the lung, allowing it to inflate and deflate as we breathe. Normally, this process is controlled by the liver releasing more AAT, which neutralises the enzyme before it can cause too much damage to the lung.
In people with A1AD there is a fault in a gene that is on chromosome 14. This fault causes the AAT protein to be mis-shaped and it has been shown that the molecules of the protein stick together to form “polymers”. This malformed protein becomes “stuck” in the liver and cannot get into the blood stream.
To have A1AD means that you have inherited a faulty gene from both parents so that both chromosome 14’s have the faulty gene. This is the highly deficient state where blood levels show that less than 20% of normal levels are circulating in the blood. There are many subtle differences in the gene that makes AAT. It is said to be “polymorphic” and up to 100 different types of AAT have been documented.
Scientists developed a way of showing these differences by using a gel plate to document the way the different varieties moved when subjected to an electric charge. They gave different letters to the different types of Proteinase Inhibitor they found, the Pi system. It was found that the least effective and most malformed AAT was the Z type. So, when a person is tested for A1AD the lab performs what is called a “Phenotype”, which shows what sort of AAT the patient has. If you have two normal genes then the patient is described as PiMM, where the two “M’s” mean that both genes for A1AD are normal and are producing normal AAT.
In the highly deficient patient the results are likely to be PiZZ, showing that both genes for AAT are producing the near useless Z type. Without the protection of AAT the lung tissue can become slowly damaged by repeated infections and the unopposed neutrophil elastase that the white cells have released. Smoking causes these white cells to rush to the lungs so that anyone who is highly deficient, PiZZ, will be at a huge risk of developing severe, progressive emphysema at an early age.
In Northern Europe the commonest type of deficiency is PiZZ, the worst sort. In Denmark, a country with a small, very inbred population the chance of having full-blown A1AD is 1:1600, which in Denmark makes it twice as common as Cystic Fibrosis. It is not know what the frequency is in the UK as no assays have been carried out but it’s thought to be around 1:5000.
Another quite common variety of the gene is given the label “S” type. This particular variety (allele) seems more common in Spain and Italy and is also found in Latin American Countries. Being PiSS (both genes S type) does not appear to cause as much disease as being PiZZ. although it does increase the risk of emphysema in smokers.
So, we have seen that people with A1AD cannot produce enough of the protective protein, AAT and are at a high risk of developing severe emphysema, often in their forties. This is by far the most common disease caused by the deficiency.
For some people the accumulation of misfolded AAT protein causes cirrhosis of the liver which can be life threatening. It is not understood why only some PiZZ individuals develop severe liver disease but it is suspected that either another gene is involved or perhaps some other liver injury like an unknown hepatitis virus. This form of liver disease is usually seen in older people with A1AD. Around 20 babies a year are born showing symptoms of neo-natal liver disease caused by A1AD. Most of these will improve and many show only mild liver abnormalities by the time the reach puberty. Perhaps two a year will require a liver transplant whilst still an infant. This should not be confused with the “jaundice” often seen in neo-nates as this is not a problem and soon fades. These few babies are very sick indeed and will die if not treated.
In rare cases a skin condition known as Panniculitis can develop which is an inflamation of the panniculus, the layer of fatty and fibrous tissue beneath the outer layers of our skin. Panniculitis due to alpha-1 was first detected by physicians in France in 1972 where they described a young woman with a severe deficiency of alpha-1 antitrypsin who developed characteristic red nodules and painful skin ulcers.
