How do you get Alpha-1?
 Genetic disorders fall into several categories. Some are caused by a single mistake (mutation) in the DNA code. Disorders like Cystic Fibrosis, Sickle Cell Anaemia, Huntingtons and Alpha-1 are all caused by a single gene (obviously different single genes for each disorder). Others are caused by a combination of genetic mistakes. Some disorders are “dominant” and others “recessive”.
Genetic disorders fall into several categories. Some are caused by a single mistake (mutation) in the DNA code. Disorders like Cystic Fibrosis, Sickle Cell Anaemia, Huntingtons and Alpha-1 are all caused by a single gene (obviously different single genes for each disorder). Others are caused by a combination of genetic mistakes. Some disorders are “dominant” and others “recessive”.
Huntingtons disease, which causes devastating destruction of the brain, is “dominant”. This means if either of your parents have the disease then you have a 50/50 chance of having the faulty gene. If you have the faulty gene you will develop the disease. Alpha-1 and Cystic Fibrosis are examples of “recessive” genetic disorders. To have A1AD you have to have inherited the faulty gene from both parents. These people would have been the first to have A1AD.
What are chromosomes?
Chromosomes are tightly packed with long stands of DNA. We inherit 23 chromosomes from each parent, a total of 46 in all. It has been said that were we only to have one set of chromosomes we would die very rapidly as most “‘sets” carry some mistakes. Having two sets means that if one particular chromosome is faulty then the corresponding one in the other “set” can do the job that the other cannot.
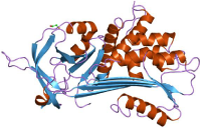
The gene that is responsible for giving the “orders” to manufacture AAT is on the long arm of chromosome 14. Some time, many thousands of years ago in Scandinavia a single person had a mutation of the chromosome 14 which caused the Alpha-1 protein to mis-fold. As this person had another chromosome 14 that produced normal AAT he wasn’t affected. However, these were very different times and family members would interbreed. This faulty gene would have spread amongst the family and inevitably interbreeding would have resulted in people acquiring TWO faulty copies of the faulty gene.
The bit that concerns us!
We’ve seen that AAT type is categorised by letters. Remember “M” type is usually normal but “S” type, and especially “Z” type produce AAT that is abnormal. Most of us who are badly affected have two copies of the “Z” type gene. Our “Phenotype” is described as PiZZ.
People who have one normal M type gene and one faulty Z type gene are “Carriers of A1AD”. They don’t have the deficiency themselves and usually have sufficient AAT produced by the M gene to protect them against lung disease. However, if they smoke they are thought to be at a higher risk of emphysema and bronchitis than a “normal” person. They have the phenotype PiMZ.
In white people of northern European extraction the number of people who are PiMZ is thought to be between 1:25 and 1:40. To be honest nobody knows because no surveys have been carried out. Any figures you see elsewhere are “guestimates”.
When two people who are PiMZ have a child there are four possible outcomes:
(1) The child could inherit both M genes and be entirely normal.
(2) The child could inherit the M gene from mum and the Z gene from dad and be a PiMZ carrier.
(3) The child could inherit the Z gene from mum and the M gene from dad, again giving the PiMZ status of carrier.
(4) The child could inherit the Z gene from mum and the Z gene from dad giving PiZZ, the “full monty” of A1AD
From that we can see that there is a 1 in four chance of the child being normal and the same chance for them having the full blown deficiency. There is a fifty/fifty chance of the child being a carrier.
PiMZ (Carrier)
For the PiZZ adult who marries a PiMM ALL offspring will be PiMZ, or carriers, because they have to get one of the two Z genes from the affected parent. For carriers (most, of course who never even know that they are carriers) any children they have will have a fifty/fifty chance of also being PiMZ.
Of course, the same is true for people who carry or have the S type of AAT. You get people who are PiMS as well as those who are PiSS and, naturally enough any mixtures like PiSZ. However, it seems true that it is only the PiZZ and some PiSZ that are at risk of developing lung disease as a direct result of the deficiency.
Testing
Testing for the level of AAT in the blood involves a simple blood pull. As we said earlier these should be in the range of 1.1g/ltr. to 2.1g/ltr. If the level is found to be lower than this reference range then Phenotyping ought to be done to determine which type of AAT your body is making. But, NHS trusts are often reluctant to do these tests because of the cost and their experiences of finding so few positives.
There is another problem with testing only levels without Phenotyping as well. AAT is what is called “acute phase reactive”. This is a posh phrase to say that the levels rise if you have an infection. They also rise if you are pregnant or taking any hormones like the “pill”.
This rise only happens with M type AAT genes. So, if you are Pi MZ and you take the pill it is possible that a level only test would report that you were “normal” when you were not. It could be a similar case if a PiMZ person was tested whilst they had a bad chest infection.
